Is it unethical for GPs not to bulk-bill? Patients seem to think so

GPs who do not bulk-bill have been dubbed unethical in an annual survey of 1000 people.
The Ethics Index, an annual report by corporate ethics thinktank the Governance Institute of Australia, has historically shown that patients have positive opinions of GPs.
In this year’s edition, GPs still ranked the fifth most ethical professional group, behind nurses, pharmacists, ambulance workers and firefighters.
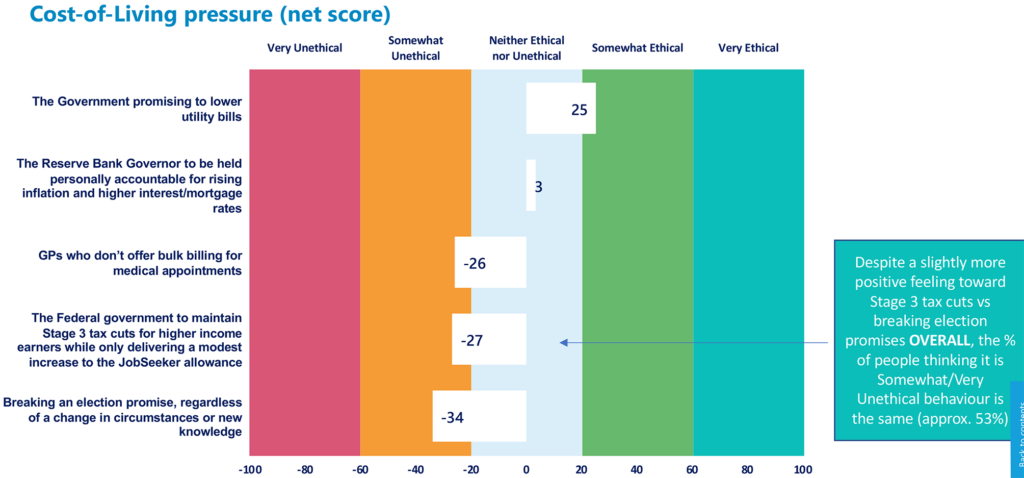
But for the first time, the poll asked people to rate the ethical behaviour of GPs who did not offer bulk billing for medical appointments as part of a new segment on the cost-of-living crisis.
The online survey by polling company Ipsos gave the options of very unethical, somewhat unethical, somewhat ethical, very ethical or neither.
Private billing GPs received a net score of –26, meaning somewhat unethical.
The survey did not go into the arguably more interesting questions around who GPs chose to bulk-bill — whether they bulk-billed all comers or only patients without the means to pay.
The bulk-billing rate for all face-to-face Level B consultations fell to 72% last financial year.
Adjunct Clinical Professor Karen Price, who called for GPs to abandon universal bulk-billing during her RACGP presidency, said the survey results highlighted patient misperceptions of the Medicare system.
“Obviously, no major supermarket does a 50% discount for disadvantaged people, yet somehow private clinics are supposed to,” she said.
For GP practices dealing with payroll tax, stagnant Medicare rebates and rising utility costs, Professor Price said the foremost ethical consideration was staying viable.
“The government has a social contract with the electorates, and they’ve failed to consider the needs of particularly marginalised and vulnerable groups, and GPs have been subsidising those groups for decades.
“It’s now got to the point where we either continue that and we close the doors, or we have to charge so that we can pay our nursing staff and the cost of running the practice.”
“By some people paying a bit more for healthcare, they’re actually helping the whole community access healthcare by keeping the doors of their general practice clinics open, so each GP and each patient has to consider that.”
“You have to keep the doors open; that’s the more ethical decision.”
Away from bulk-billing, the 2023 Ethics Index found that perception of GPs’ ethics remained steady, but they had been leapfrogged in the professions ranking because of surging positive opinions of pharmacists and emergency services.
For organisations, the AMA remained highly rated for ethics, while the only organisation to go backwards was the Governance Institute of Australia, which ran the survey.
More information: Governance Institute Ethics Index 2023

