‘If you do no harm you do nothing’: The story of a medical revolution

Blood stem cell transplants have transformed the care and lives of millions.
But the origins of this medical revolution are rooted in a dangerous experiment.
The following excerpt comes from a new book, Flesh Made New: The Unnatural History and Broken Promise of Stem Cells, cowritten by Professor John Rasko, haematologist and professor of medicine at the University of Sydney.
It tells the remarkable story of Dr Don Thomas and his efforts to make bone marrow transplantation safe.
In mid 1950s, soon after starting work at a hospital in New York, Dr Don Thomas — with the help of his wife, Dottie, and his research partner, Joe Ferrebee — began performing bone marrow transplantations on patients with blood diseases such as leukaemia.
This inspired others to follow suit, leading to an early boom in the procedure.
The results, however, were dismal.
Patient after patient died and, by 1963, when Don and Dottie moved to Seattle, Washington, the field had collapsed.
At the University of Washington, Don experimented on dogs to solve the problem of tissue typing.
By early 1969, Don decided it was finally time to try on people what he and his Seattle team had learnt by working with dogs.
Their first patient was a 46-year-old man with leukaemia named Bill.
He had five potential marrow donors: his parents, two sisters and one brother.
All of them were tissue typed twice, first in Don’s lab, using antisera supplied by the immunologist Dr Bernard Amos at Duke University in North Carolina and again in the lab of the scientist Dr Paul Terasaki (PhD) at the University of California.
Both these researchers were world authorities on human tissue typing and both labs identified one of Bill’s sisters as a good — but not a great — match.
So in March 1969, Bill was driven to the ex-military bunker that housed Don’s powerful X-ray machines — dubbed the “cobalt bombs” — and his research dogs.
As there was no lift, Bill was carried down the stairs on a stretcher.
Don later admitted that the place made a frightening first impression.
“As the patient was carried down into the radiation area, all of the dogs would begin to howl, thinking it was feeding time.
“To the patient it must have been something comparable to a descent into hell.”1
Placed under the cobalt bombs, Bill received lethal radiation for five nausea-filled hours, with several brief breaks to help him cope.
In the meantime, his sister was unconscious on an operating table at the hospital, having marrow extracted from a hundred points along her breastbone and hip.
When the radiation was complete, Bill was raced to the hospital, where he received his sister’s marrow intravenously.
In the annals of science, this case is considered a milestone, proof that bone marrow transplantation had finally come of age.
However, clinically speaking, it was a failure. Everything went to plan for the first month and a half. Bill’s marrow graft took, saving him from the dire effects of radiation.
He suffered an awful body rash due to graft-versus-host disease (then known as “secondary syndrome”), but methotrexate brought it under control.
Best of all, his leukaemia disappeared entirely.
But then Bill fell sick again, developing a fever, diarrhoea and finally pneumonia. He died 56 days after the treatment.2
His doctors assumed that Bill’s graft-versus-host disease had returned, but the autopsy said otherwise.
The real culprit was cytomegalovirus (CMV), a virus that in ordinary circumstances would have gone unnoticed.
But in Bill’s immune-compromised body, it had run wild.
“It was our very first case of CMV,” says Don’s colleague, Dr Rainer Storb.
The team were not prepared for it because dogs don’t get CMV.
“It was very devastating, and all of a sudden we had a new problem.”3
For a few months after a marrow transplant, patients are extremely susceptible to all kinds of bacteria, viruses and fungi.
Infections that barely trouble someone who is healthy turn into stone-cold killers. The Seattle team found that out the hard way.
As Don Thomas recalled decades later: “We learned about all the infections that AIDS patients get long before AIDS came along.”4
In their efforts to develop bone marrow transplantation, it seemed that Don and his colleagues had cleared one hurdle only to trip immediately over another.
Obviously, they had to do more to control infections.
For that, they needed better hospital facilities, including single-bed isolation rooms. They needed special air-flow systems to reduce the risk of airborne diseases.
They needed their own dedicated nursing staff trained to deal with immune-compromised patients.
In fact, Don had been working hard to acquire all these things. After years of planning and grant writing, he finally got a special six-bed unit, properly equipped and staffed, on the seventh floor of the Public Health Service Hospital.
Unfortunately, it hadn’t been ready in time for Bill, opening a few months after his death.5
(While such facilities did help fight infections, the real game-changer only came later with the appearance of better antibiotics and antivirals.)
By the end of the 1960s, improvements in tissue typing and patient care had ushered in a new era in medicine.
It dawned slowly enough, its first bright signs appearing not in Seattle, but in the Midwest.
Read more: Two stem-cell transplants better than one in neuroblastoma
On 9 November 1968, two teams of researchers — one led by Robert Good in Minnesota, the other by Fritz Bach in Wisconsin — announced very similar successes with bone marrow transplantation.
Papers across the United States soon carried the news.
Oddly enough, the two patients were both young boys named David, both had similar immune diseases, and both received marrow (twice) from their sisters, both of whom were eight years old.
However, the most important parallel was that both boys — David Camp and David Zeissett — were cured and lived for decades after the procedure.6
The two Davids hadn’t needed radiation or chemotherapy, for they’d not had cancerous cells to kill. Or even a functioning immune system to knock out in preparation for the graft.
All they’d needed was new marrow from their sisters. That made them a lot easier to treat than patients with blood cancers like leukaemia, as the Seattle team discovered.
“We lost probably the first 10 patients from various causes,” says Rainer Storb. “So the initial experience was very negative.”7
After that, though, they had some successes. For Rainer, the most memorable was a boy with advanced leukaemia, six or seven years old and the son of a physician.
“He survived and actually lived, as I recall, another 20 years.”
But successes were few and far between.
With such a patchy track record, Don faced plenty of resistance.
“[W]hen we started in again [treating] people, we were very heavily criticised,” he said.
“There were very many responsible people who said this shouldn’t be allowed to go on, because our success rates, in the past, had been so poor.”8
Even Don had his doubts.
He worried about whether he was doing the right thing: “The Hippocratic Oath says ‘Do No Harm’. But if you do no harm, you do nothing.”9
Don was on the horns of a moral dilemma.
On the one hand, his attempts to cure patients often shortened their lives and added to their suffering.
On the other hand, without his efforts, they had no hope of survival at all.
In the end, Don figured that, so long as there was a real chance of success, and so long as his patients understood the risks, he should proceed.
It wasn’t an easy decision to stick to.
“We put these people through hell, horrible pain and agony,” said Alexander Fefer, another of Don’s Seattle colleagues.
“It took a tremendous amount of chutzpah, arrogance, hubris — whatever you want to call it — to say we should continue.”10
But continue they did, through some very tough times.
When the Federal Government, in 1972, threatened to close public hospitals across the USA, including the one that housed Don and his staff, the future looked bleak indeed.
They scrambled to find temporary space at another hospital and spent the next few years in limbo.
Finally, in 1975, they moved into their new home at the newly built Fred Hutchinson Cancer Research Center. There at ‘The Hutch’, Don was head of oncology and had superb facilities at his disposal.11
Between 1971 and 1975, Don’s team treated 100 leukaemic patients at various hospitals in Seattle and then published a paper summarising their results.12
It did nothing to silence the critics.
On the contrary, many thought they were just parading their failures. At the time of publication, 83 of the 100 patients had already died and four of the survivors had relapsed. Soon the number of those left alive fell from 17 to 12.
According to Don: “People were saying, ‘Well, you know, only 12 out of 100 isn’t worth all this effort and expense.'”
Don read those figures very differently:
“They were all in the end stages of leukemia. To have 12 of them become long-term survivors was, to me, very impressive … it meant, if we can do this with patients with far-advanced disease, even if there’s no other progress, we should be able to do much better if we do it much earlier, before they get to the end stage of the disease.”13
Eight of those 12 patients were still alive and disease-free 20 years later, which is long enough to be officially declared ‘cured’.14
Eight out of 100 may sound underwhelming, but it represented a quantum leap forward. Leukaemia was no longer a death sentence.
There was now reason for hope, a real chance of being cured, something previously impossible.
The task ahead was to increase the odds of survival. Initially, bone marrow transplantations were given only to those near death, but, as the number of successes grew, it became acceptable for doctors to treat patients sooner, while they were still in good shape.
This further improved survival rates, which in turn made doctors bolder still. Bone marrow transplantation was gaining acceptance.
Not just as a treatment for leukaemia but for a range of blood diseases.
The rise of bone marrow transplantation is easy to chart. From 1957 to 1970, the total number performed was just 275. After that, however, it skyrocketed, reaching a total of 10,000 in 1986.
Around then, researchers realised that the bone marrow’s most important ingredient — its blood-forming stem cells — could be harvested directly from the blood.
By the end of 2012, blood stem cell transplants had hit the one-million mark.15
What had begun in the 1950s as a dangerous and doubtful experiment attempted here and there by a handful of ambitious researchers had become a routine medical procedure, practised in hospitals around the world. It was nothing short of a medical revolution.
Nobel Prize
Bone marrow transplantation was the world’s first stem cell therapy, but that’s not how it was initially understood.
When Don was in Cooperstown, and for a while after moving to Seattle, he didn’t really consider himself a stem cell scientist.
He started learning how to harness blood stem cells before he or anyone else really knew what they were.
We often imagine scientific progress to be a series of great discoveries made by the brilliant few, that for each advance, there is a genius or two blessed with a eureka moment.
It’s an attractive storyline, and we find it endlessly repeated in the news, but science often doesn’t work that way.
After Don won the Nobel Prize in 1990, journalists would always ask him what his breakthroughs were.
It was a question he dodged in this manner: “I always say there aren’t any breakthroughs. It’s always a step-by-step process.”
And more precisely: “You get interested in something, and one problem crops up. If you’re lucky, you can solve this, but it discloses three more problems. So you’re led forward by curiosity.”16
To some extent, the idea of genius is reinforced by the Nobel Prize itself, which is always awarded to exceptional individuals – a maximum of three for each category.
When the awards were originally set up in 1901, there were still some individual scientists making big discoveries.
But they were an endangered species, soon to be replaced by teams of researchers pooling their resources.
As science became increasingly complex, scientists found their own areas of expertise shrinking and had to rely on each other’s assistance ever more.
No wonder that scientific articles often list a dozen or more authors nowadays. In recent years, there have even been articles with more than 1000 authors!
Perhaps that’s why Nobel Prize winners like Don devote much of their acceptance speeches to acknowledging the work of others, near and far.
Aside from being suitably humble, they’re correcting the romantic bias built into the proceedings.
Don’s Nobel Prize and his subsequent reputation as ‘the father of bone marrow transplantation’ provide a case in point.
He was a terrific scientist, but not a genius standing head and shoulders above his contemporaries.
Although he was in the thick of a medical revolution, he didn’t do anything very revolutionary.
What discoveries he made were modest, the result of collaborative work all directed towards practical ends: ultimately, the treatment of patients.
In any clinical advance, success depends on an accumulation of knowledge, but also an accumulation of practices, technologies and institutional arrangements.
For blood stem cell transplantation to become a medical mainstay, innumerable things had to coalesce: radiotherapy, chemotherapy, cell culturing, tissue typing, blood banking, the development of drugs to fight infection and suppress the immune system, and countless measures to support patients through the whole ordeal.
Don was responsible for a tiny fraction of that. To single him out for a Nobel Prize was thus a somewhat arbitrary decision.
Despite this, we think that Don was well chosen.
No one worked longer or harder on bone marrow transplantation. No one was more central to its development.
There were many teams engaged in this field, but those led by Don took an especially broad and systematic approach, always stepping back and forth between the lab and the clinic, always translating scientific results into medical practice.
If Nobel Prizes were awarded to teams, the obvious contenders would be those that Don led in Seattle, first at the University of Washington and then at The Hutch.
But since the prize always goes to individuals … well, no one was more deserving than Don Thomas.
His old Cooperstown colleague Harry Lochte reckons that Don wasn’t much interested in awards. His focus was always on his work.
Harry tells a story about taking his wife and grown-up daughter to visit Don at The Hutch. They were all chatting away when Harry’s daughter asked to see Don’s Nobel Prize.
He was more than happy to oblige and started to search his office for the chunky gold medallion, riffling through one drawer after another. ‘It’s around here somewhere,’ he said.
Harry can’t remember whether Don actually found it, but he is sure that, had Dottie been around that day, she’d have known exactly where to look.17
Flesh Made New: The Unnatural History and Broken Promise of Stem Cells is written by Professor John Rasko, professor of medicine at the University of Sydney, and writer and historian Carl Power.
To order a copy, click here.
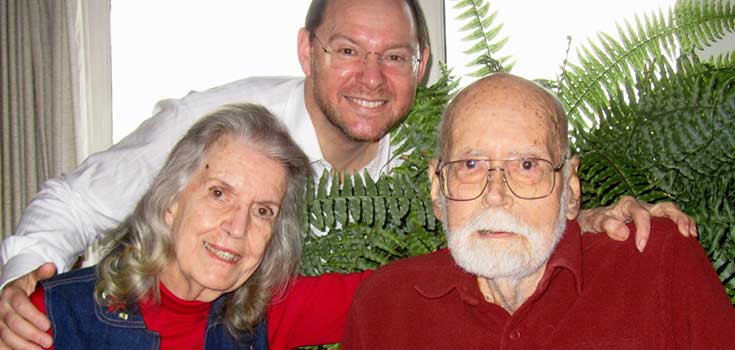
Professor John Rasko with Dotti and Dr Don Thomas — the ‘mother and father’ of bone marrow transplantation — in the late 1990s.
Professor Rasko trained at the Fred Hutchinson Cancer Research Center which was established in Seattle, Washington.
References on request from paul.smith@ adg.com.au